One way for insurers to reduce health care costs is to restrict patient access to only lower cost providers. This phenomenon is known as narrow networks. On the one hand, narrow networks can promote efficiency by driving down provider price and directing patients to the highest value physicians. Alternatively, if insurers use narrow networks to direct patients to providers based solely on cost, the quality of care patients receive in narrow networks may decline.
What share of silver plans in health insurance exchanges use narrow networks? This is the question Polksy and Weiner (2015) address in their issue brief. They use data from 1,065 unique silver plans sold in all states (plus DC) as provided by HIX Compare to identify the size of different provider networks for each insurer. They found that:
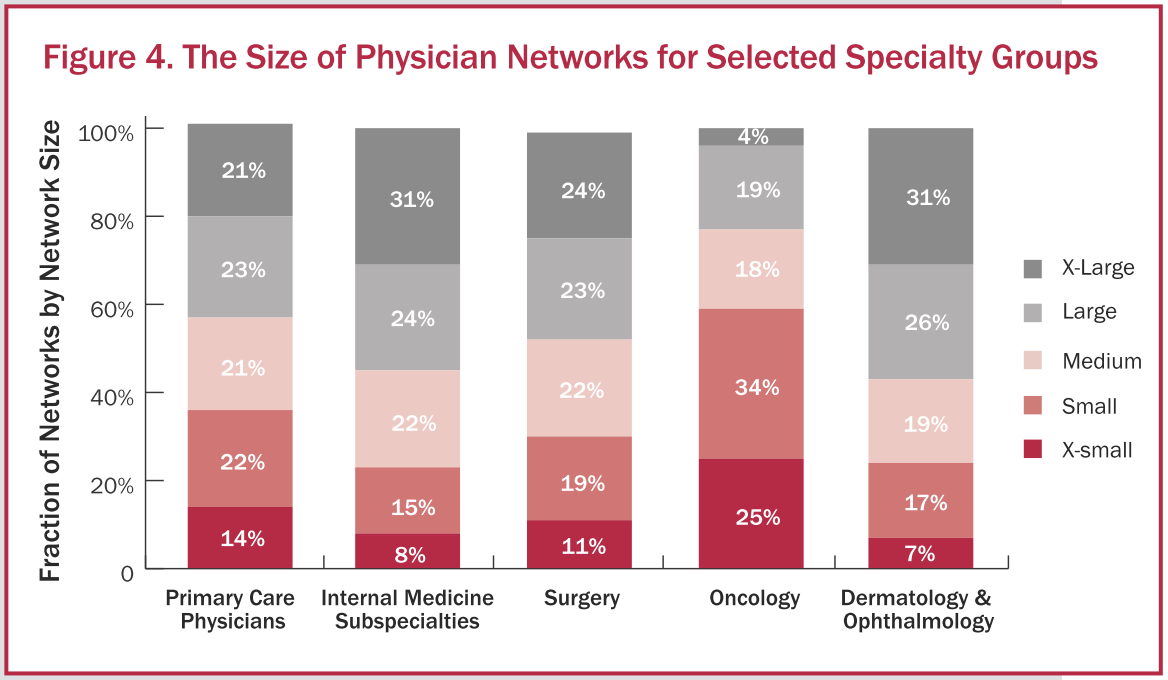
By our measures, 41% of networks are small or x-small: 11% of networks are x-small, meaning they include less than 10% of office-based practicing physicians in the area and another 30% are small, including between 10% and 25% of physicians. At the other end of the spectrum, 11% are x-large, which we define as networks including more than 60% of physicians.
As the figure below shows, although only 36% of networks are narrow with respect to primary care physicians, for oncologists 59% of networks are narrow. Thus, access to high cost oncology services is more limited. It is not clear whether narrow networks are moving patients towards oncology specialist or simply reducing patient access to care. Additional research is needed to determine how narrow networks affect patient outcomes, particularly for patients with cancer.
Source:
- Dan Polsky, PhD and Janet Weiner, MPH. The Skinny on Narrow Networks in Health Insurance Marketplace Plans. RWJF Issue Brief, June 2015.