In my previous work, I have examined regional variation in Medicare and Medicaid costs through reports to the Institute of Medicine and publications in peer-reviewed journals. We found significant variation in health care costs across regions, that high-cost regions tended to remain high cost over time, but that a region that is high-cost for treating one medical condition may not be high cost for another medical condition.
A new paper in Health Services Research by Krinsky et al. (2016) examines the causes of regional variation in Medicare inpatient cost between 1987 and 2013. In the current Medicare inpatient reimbursement system–the Inpatient Prospective Payment System (IPPS)–hospitals are paid:
…based on patients’ diagnosis related groups (DRGs), and it also compensates hospitals for exceptionally costly patients through outlier payments. While each DRG is assigned a base price that applies to all U.S. hospitals, hospitals receive payment adjustments designed to account for differences in area wages, care for low-income patients under the disproportionate share hospitals (DSHs) program, and the indirect costs associated with graduate medical education (IGME), among other adjustments.
The size of these adjustments have varied over time. For instance, the the Affordable Care Act (ACA) “reduced DSH payments by 75 percent and introduced a new uncompensated care adjustment, beginning federal fiscal year (FY) 2014.”
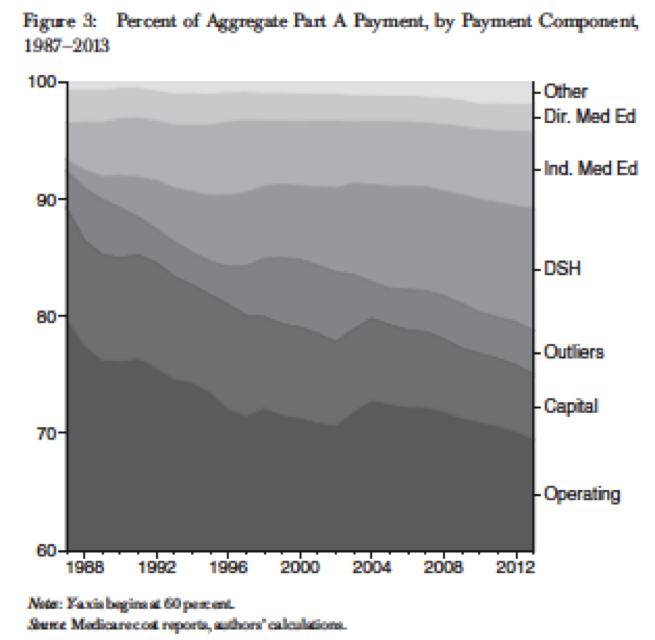
Using Medicare hospital cost reports, Krinsky et al. (2016) decomposed Part A payments into seven components: operating, capital, outlier, DSH, IGME, DGME, and an “other” category. The authors measure the share of these adjustment payments relative to the base DRG payment.
The studies find that a growing share of Medicare payments for Part A inpatient care are for payment adjustments rather than the base DRG payments (see figure below). As the adjustments are more likely to vary across regions, we see that over time, variability in Medicare hospital reimbursement rates has increased over time as well.
The authors summarize the results as follows:
Over the 27 years of the IPPS covered in our study, adjustments represented a large and increasing share of Medicare expenditures for acute inpatient care. The highest rates were paid to hospitals that received large payments both for DSH and medical education. Community hospitalsreceived the lowest rates.
The authors also measure variation in reimbursement within hospital referral regions (HRRs). However, use of HRRs is not the best approach. The Medicare Hospital Wage Index–used to adjust hospital payments for regional differences in labor costs–is defined by metropolitan statistical area (MSA) and rest of state areas. Whereas HRRs are agglomerations of ZIP codes, MSAs are agglomerations of counties. Thus, there may be heterogeneity in reimbursement rates within HRR by design due to CMS policy. Nevertheless, the finding that adjustments make up a larger share of IPPS reimbursement is certainly an interesting one.
Source:
- Krinsky, S., Ryan, A. M., Mijanovich, T. and Blustein, J. (2016), Variation in Payment Rates under Medicare’s Inpatient Prospective Payment System. Health Services Research. doi: 10.1111/1475-6773.12490